Define pleura.
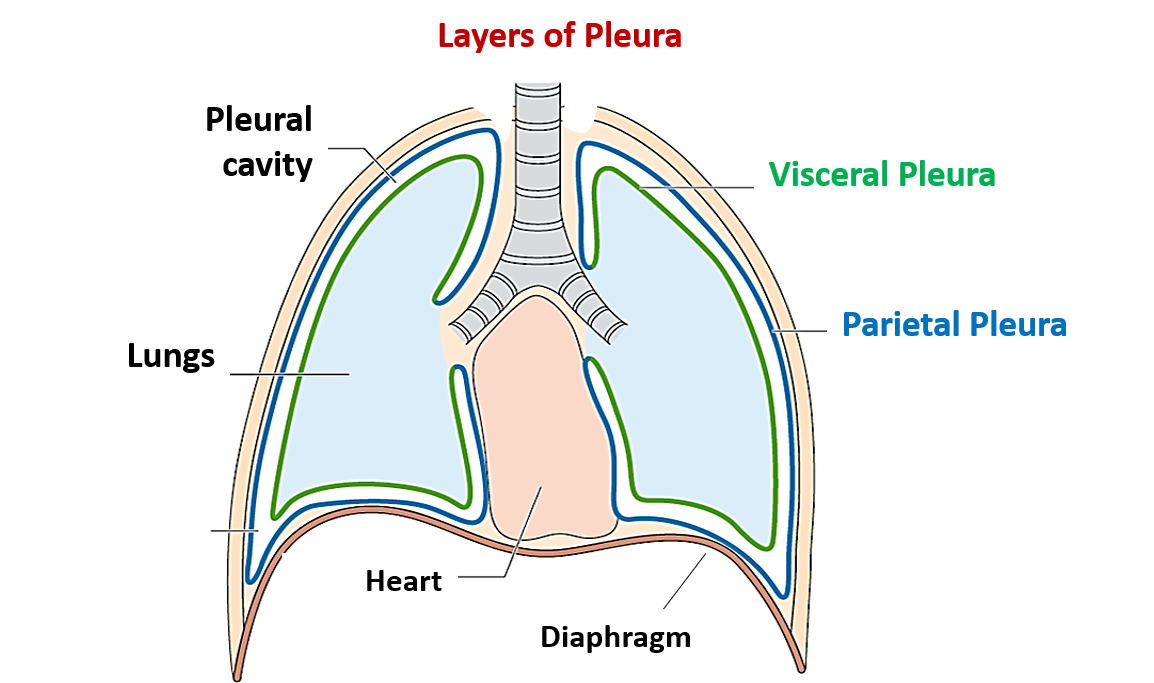
Pleura is a serous membrane lined by mesothelium(simple squamous epithelium) that is present as a closed sac around the lungs. It comprises of two layers, outer parietal and inner visceral layer.
Define peural cavity.
Pleural cavity is a closed potential space between the parietal and visceral layers of pleura. It normally contains only a thin film of serous fluid which is secreted by the pleura. The space becomes apparent if there is accumulation of air (pneumothorax), blood (haemothorax) or pus (empyema).
What are the characteristic features of visceral pleura?
Characteristic features of visceral pleura:
- It is the inner layer of the two layers of pleura.
- It is tightly adherent to the outer surface of lung .
- It also lines the fissures of the lung.
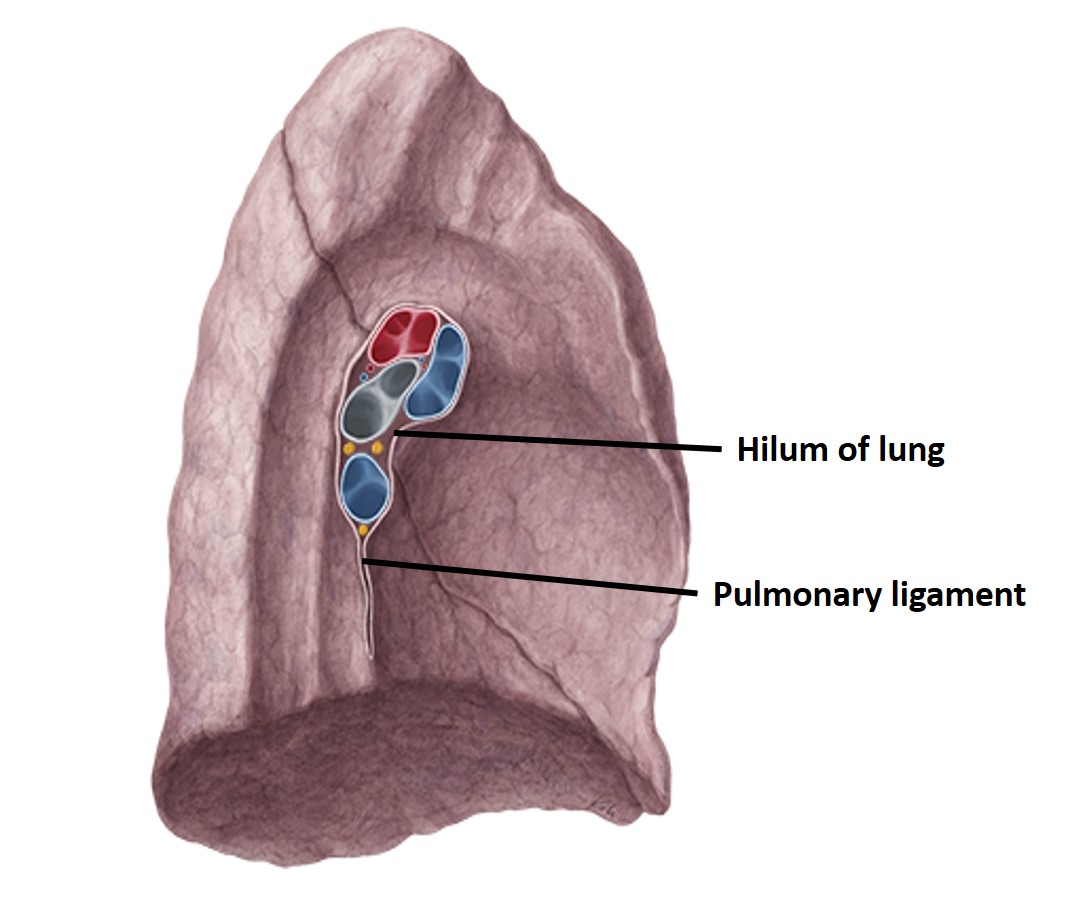
- It does not cover the hilum of the lung and the area along which pulmonary ligament is attached.
- It develops from the splanchnopleuric layer of the mesoderm.
- It is innervated by the autonomic nervous system and is therefore insensitive to pain.
- It is continuous with the parietal layer at the root of lung.
What are the characteristic features of parietal pleura?
Characteristic features of parietal pleura
- It is the outer layer of the two layers of the two layer.
- It lines the corresponding half of the thoracic wall separated from it by endothoracic fascia(areolar tissue), covers the thoracic surface of diaphragm and the mediastinum.
- It develops from the somatopleuric layer of the mesoderm.
- It is innervate by the somatic nervous system and is therefore sensitive to pain.
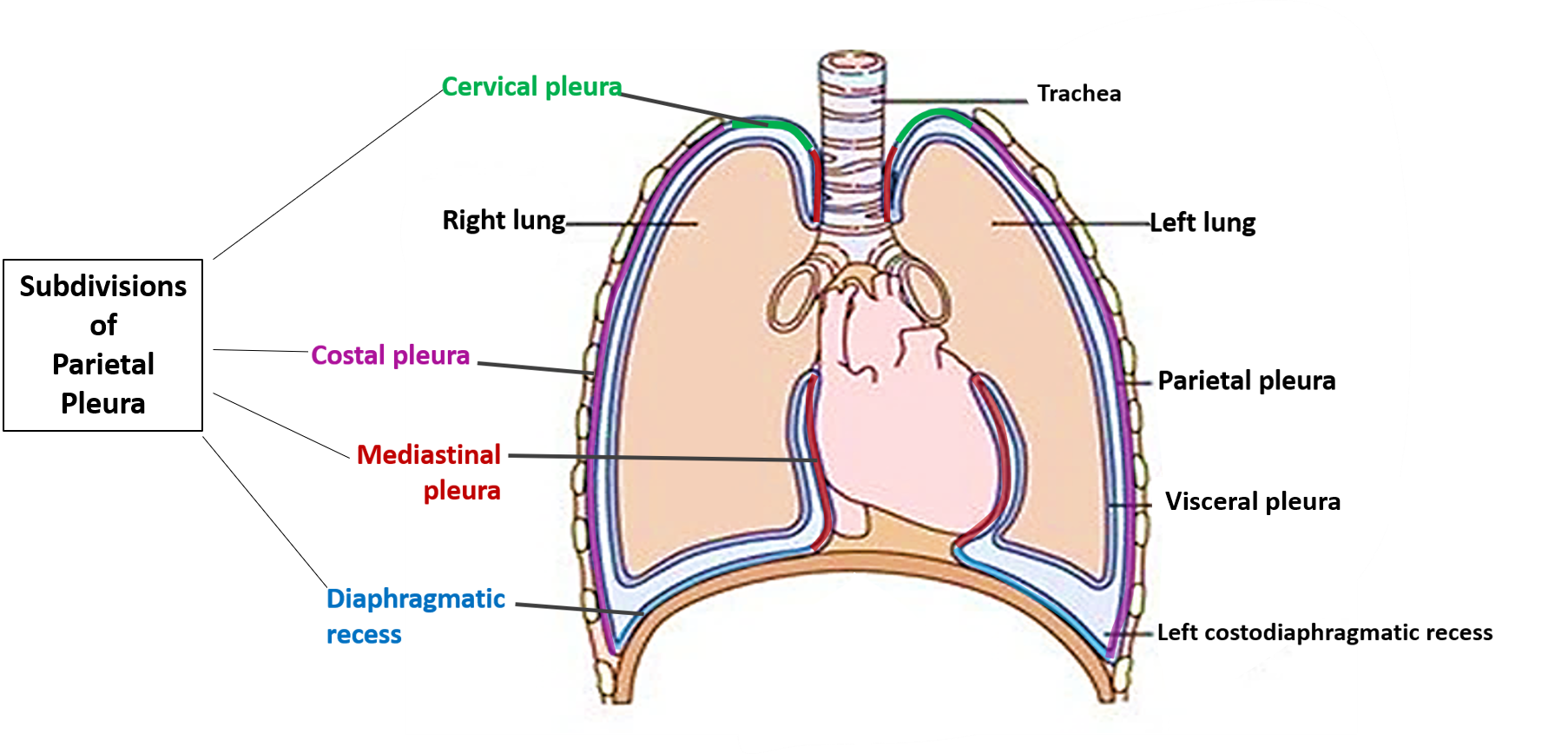
What are the various subdivisions of parietal pleura?
Parietal pleura is given different names that correspond to the structures with which it is associated.
- Cervical: Dome shaped pleura extending into the neck (summit is 2.5cm above the clavicle)
- Costal: Lines the ribs and intercostal spaces.
- Diaphragmatic: Pleura covering the diaphragm
- Mediastinal: Pleura covering the mediastinum.
Name the sites where the parietal pleura extends beyond the thoracic cage.
Sites where the parietal pleura extends beyond the thoracic cage and is in danger of being injured.
- Above the medial 1/3rd of the clavicle on both the sides
- Beyond the right xiphicostal angle
- Below costovertebral angle on both the sides.
What is pulmonary ligament and what are its functions?
Pulmonary ligament : It is the narrow fold of parietal pleura that extend below the root of lung.
Functions of pulmonary ligament are:
- Allows descent of structures of root of lung during inspiration.
- Provides dead space into which pulmonary vein can expand during increased venous return ( e.g. during exercise).
Describe the nerve supply of pleura.
Nerve supply of pleura:
- Parietal pleura: is pain sensitive
- Costal and peripheral part of diaphragmatic pleura are supplied by Intercostal nerves
- Mediastinal and central part of diaphragmatic pleura are supplied by Phrenic nerve
- Visceral pleura: Is insensitive to pain.
- Is supplied by autonomic (sympathetic ) nerves –T2 –T5.
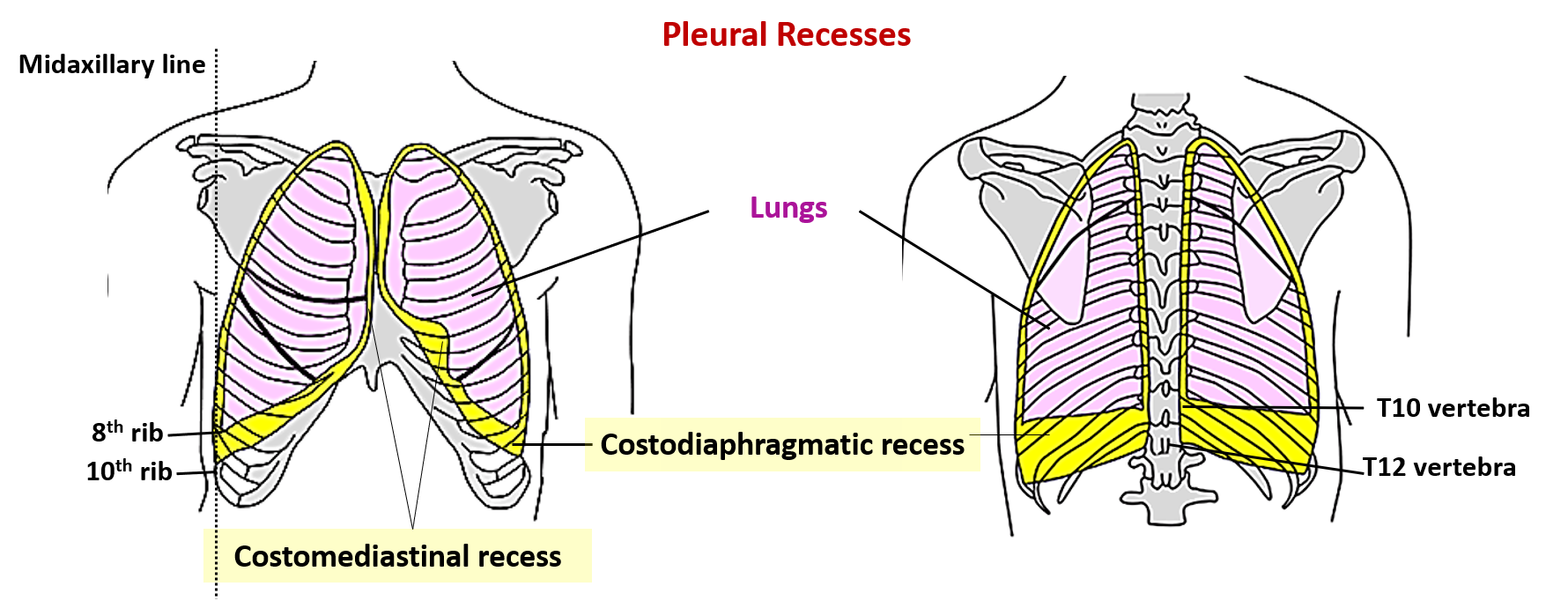
Describe pleural recesses.
Pleural recesses: Anterior and inferior regions of pleural cavities are normally not occupied by the lungs. In these regions the two layers of parietal pleura are opposed to each other resulting in presence of potenial spaces called pleural recesses . These recesses allow expansion of lungs during inspiration. The two recesses of the pleura are:
- Right and laeft costomediastinal recesses
- Right and left costodiaphragmatic recesses
Costodiaphragmatic recesss:
- Is the largest and clinically most important recess.
- Is present between the costal and diaphragmatic parts of parietal pleura.
- Is C- shaped and present between the inferior margins of the lungs and the inferior margin of the pleural cavities.
- The maximum vertical distance is 5 cm along the midaxillary line opposite to 8th-10th
- Is the most dependent part of the pleural cavity and therefore the fluid of pleural effusions first collect here.
Costomediastinal recess:
- Is present anteriorly between the costal and mediatinal pleura.
- The left costomediastinal recess is larger due to the presence of cardiac notch along the anterior border of the left lung.
Applied Aspects
Pleurisy/Pleuritis
Pleurisy is inflammation of the pleural membranes. The condition is very painful especially when a person takes deep breath. During respiratory movements, the parietal and visceral layers slide past other. Normally the pleural fluid in the pleural cavities lubricates the surfaces of these membranes.When the pleural membranes are inflamed , their surfaces become rough , the rough surfaces rub against each other and produce pain. Due to the friction between the two layers of pleura during the respiratory movements, pleural rub can be with the stethoscope.
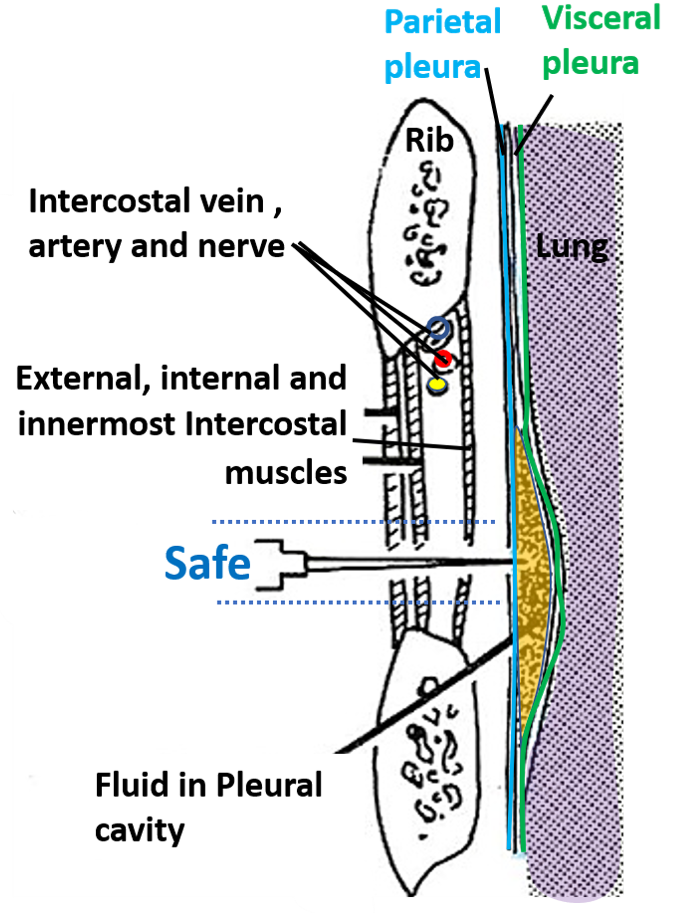
Pleural tap
It is aspiration of pleural effusion from the pleural cavity. It is usually done in the 9th intercostal space in the midaxillary line . The needle is inserted just above the upper border of the rib in the lower part of the intercostal space to avoid injury to the intercostal nerves and vessels. The needle should not be inserted below the 9th intercostal space , lest it may injure the spleen on the left side and liver on the right side.
Pneumothorax
Presence of air in the pleural cavity is known as pnemothorax. The increased air pressure in the pleural cavity may result in the collapse of the lung. It could be caused due to the penetrating thoracic wound, spontaneous rupture of pulmonary bulla (spontaneous pneumothorax), fractures rib, anaesthetist’s needle puncturing the pleura during stellate ganglion block, in making a loin incision to expose kidney, to perfom adrenalctomy or to drain a subphrenic abcess.
Tension pneumothorax is a condition in which the ruptured tissues of thoracic wall form a valve that permits air to enter the pleural cavity upon inspiration, but does not allow air to escape during expiration and therefore greatly increases the pressure inside and pushing the mediastinal structures to the opposite side.
Pleural effusions
The excessive accumulation of fluid in the pleural cavity is called pleural effusion. It is usually due to inflammation of the pleura. The progressive accumulation of fluid may cause retraction of lung towards the hilum and may displace the mediastinum to the opposite side. The fluid may be in the form of:
- Blood – Haemothorax
- Pus – Pyothorax/empyema
- Lymph – Chylothorax
Referred pain in inflammation of pleura
In inflammation of the mediastinal and central part of diaphragmatic pleura, the pain is referred to the root of neck and the shoulder region as these parts of pleura are supplied by phrenic nerve (C3,C4,C5) and the skin at the above mentioned sites is innervated by the same spinal segments via supraclvicular nerves (c3, C4).
When lower costal or peripheral part of diaphragmatic pleura are affected, the pain may be referred to the anterolateral abdominal wall along the distribution of lower intercostal nerves which also innervate the anterior abdominal wall.

This site proved very helpful to me.
It helped me for better review of my concepts.
I want to follow this…
Oops good
Wawooo am relieved of anatomy. Am grateful.