What are the characteristic features of coronary arteries?
WATCH VIDEO ON CORONARY ARTERIES [CLICK HERE]
Coronary arteries are:
- highly enlarged vasa vasorum that supply the heart.
- the only arteries that get filled up during diastole of the
heart. - the only branches of ascending aorta.
- functional end arteries i.e. the anatomical anastomosis
exist between the branches of coronary arteries,
however they are inadequate to compensate for the sudden
occlusion.
Describe the arterial supply of heart .
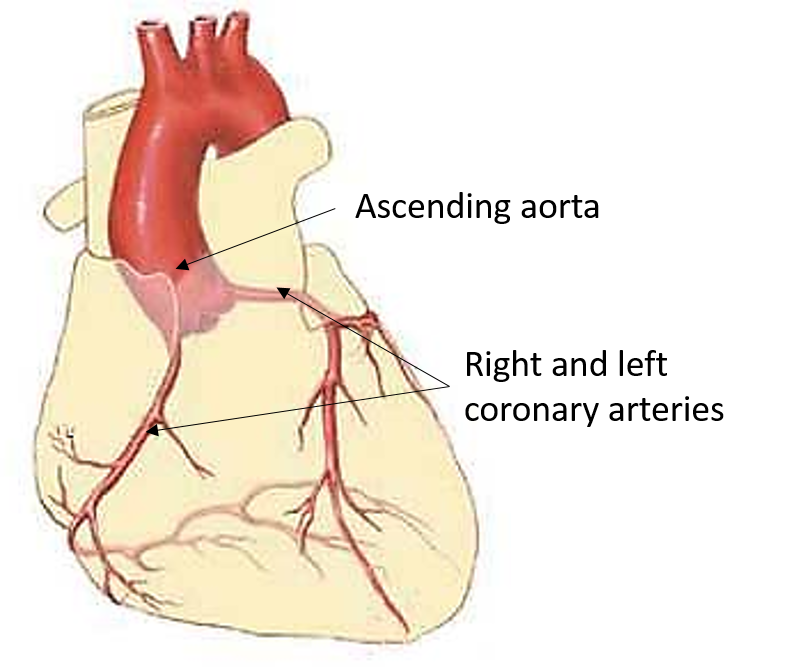
The heart’s arterial supply is derived from the right and left coronary arteries which are the branches of ascending aorta.
Right coronary artery
Origin: It arises from right ( anterior ) aortic sinus.
Course:
- Passes forward between the pulmonary trunk and the right auricle.
- Descends to the right in the atrioventricular sulcus (coronary sulcus).
- Turns posteriorly at the junction of right and inferior border.
- Continues along the posterior part of coronary sulcus to anastomose with the branch of left coronary artery.
Branches
- Right conal artery
- Artery to SA node (65% of cases)
- Right marginal artery
- Posterior interventricular branch –gives a branch to AV node ( 90% of cases).
- Unnamed branches to right atrium and right ventricle
Areas supplied
- Most of the right atrium.
- Right ventricle except the area adjoining anterior interventricular groove.
- Left ventricle adjacent to the posterior interventricular sulcus.
- Posterior 1/3rd of the interventricular septum.
- SA node in 65% of the cases.
- AV node and bundle of His, except left branch of bundle of His.
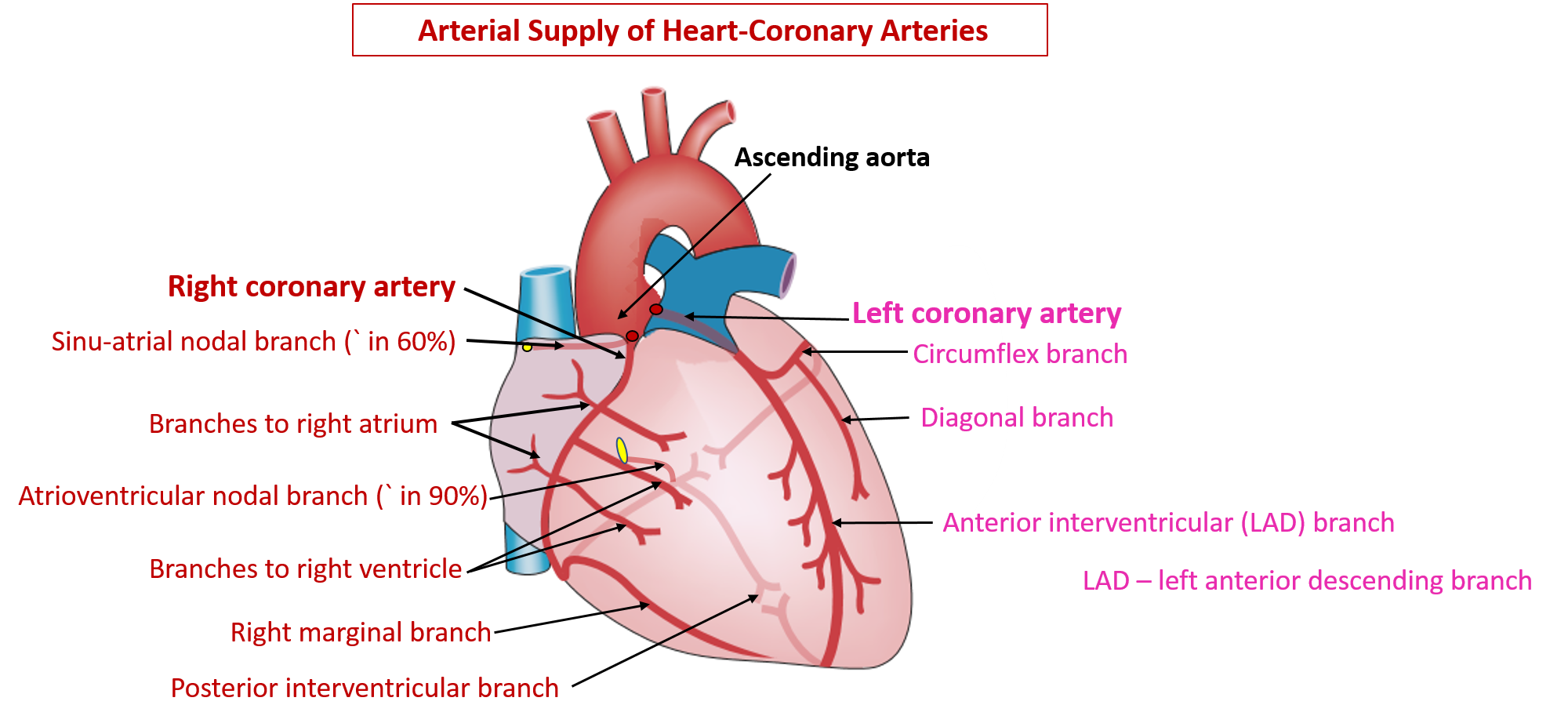
Left coronary artery
Origin: It arises from left ( left posterior ) aortic sinus.
Course:
- It passes first behind and then to the left of the pulmonary trunk to reach the left part of the atrio-ventricular sulcus
- Divides into anterior inter-ventricular and circumflex branches
- The circumflex branch represents the continuation of the left coronary artery and it turns round the left border of heart and continues along the posterior part of coronary sulcus to anastomose with the branches of right coronary artery.
Branches
- Left conal artery
- Anterior interventricular artery
- Circumflex artery
- Diagonal artery
- Unnamed branches to left atrium and ventricle
Areas supplied
- Left atrium
- Left ventricle except the area adjoining posterior interventricular groove.
- Right ventricle adjacent to the anterior interventricular sulcus.
- Anterior 2/3rd of the interventricular septum.
- SA node in 35% of the cases.
- AV node in 10% of the cases.
- Part of the left branch of bundle of His.
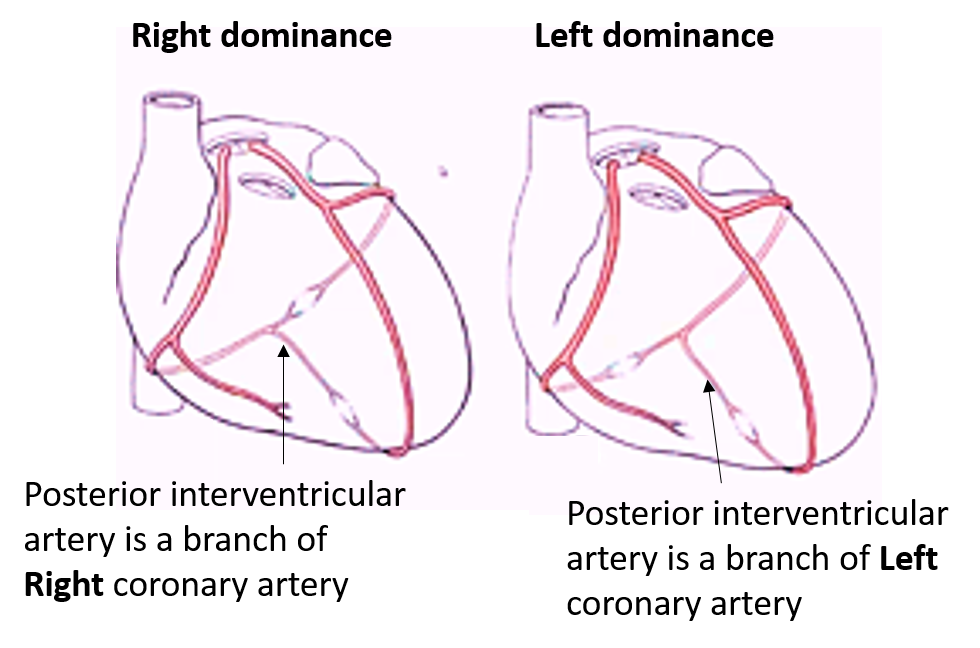
Describe briefly the ‘cardiac dominance’.
Coronary artery dominance: The artery which gives rise to the posterior interventricular artery (posterior descending artery (PDA) arises determines the coronary dominance.
- If the posterior interventricular artery is a branch of right coronary artery then the coronary circulation is said to be “right-dominant”.
- If the posterior interventricular artery arises from circumflex artery, a branch of the left artery, then the coronary circulation is “left-dominant”.
- If the posterior interventricular artery arises from both the right coronary artery and the circumflex artery, then the coronary circulation is “co-dominant/balanced”.
Approximately 70% of the general population are right-dominant, 20% are co-dominant and 10% are left-dominant.
Applied Aspect
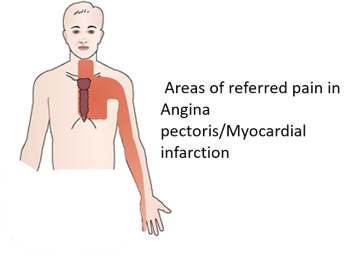
Angina Pectoris
Narrowing of coronary arteries is responsible for reduced blood flow which in turn results in decreased oxygen supply to cardiac muscle. The limited anaerobic metabolism of cardiac muscle results in built up of lactic acid which stimulates the pain receptors and as a result there is moderate to severe pain in the left precordium. The condition is called ‘angina pectoris’. The pain is often referred to left shoulder, ulnar side of left arm and forearm.
Cardiac pain due to angina pectoris or myocardial infarction is usually referred to the left precordium and medial aspect of left arm and forearm
The heart is innervated by upper four thoracic spinal segments (T1-T4). The skin over the precordium is supplied by T2-T4 spinal segments and the skin over the medial aspect of forearm and arm by T1 and T2 spinal segments respectively. The cardiac pain is therefore referred to the precordium and medial aspects of arm and forearm because of the same spinal segmental innervation.
 Prognosis of coronary disease is better in old age than in young
Prognosis of coronary disease is better in old age than in young
The coronary arteries are functional end arteries but not anatomical end arteries. Anatomically the coronary arteries anastomose with each other by their trunks , branches and mostly at the precapillary level. In case of block in the coronary artery, as a result of thrombosis or atherosclerosis, these anastomoses are not effective in young people and as a result the coronary disease can be fatal in young. The coronary disease is less dangerous in old age because the anastomoses increase and collateral channels develop with the advancement of age.

Very nice sort notes side