What is the extent of spinal cord in fetus, new-born and adults?
A. Spinal cord is the lower cylindrical part of central nervous system that is located in the vertebral canal. The vertebral column grows faster than the spinal cord, therefore, the lower end of the spinal cord gradually shifts to a higher level.
- Up to the 3rd month of intrauterine life spinal cord extends through the entire length of vertebral canal.
- At birth, the spinal cord ends at the level of L3 vertebra.
- In adults, the spinal cord extends from upper border of posterior arch of first cervical vertebra (atlas) till the level of L1 vertebra.
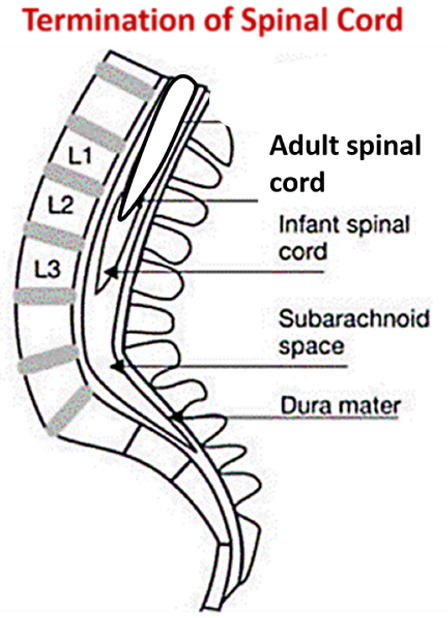
The knowledge of lower extent of spinal cord is important to avoid injury to spinal cord during lumbar puncture.
What are the functions of spinal cord?
The functions of spinal cord are:
- It transmits impulses to and from the brain to the body.
- It serves as a conduit for the passage of ascending (sensory) and descending (motor) tracts to and from the higher centers to the of brain.
- Execution of spinal reflexes, both somatic and visceral.
Name the meninges covering the spinal cord, their extent and the spaces associated with them.
The three meninges covering spinal cord from outside inside are:
- Dura mater: Spinal dura is single meningeal layer (Cranial dura covering brain has two layers – outer endosteal layer and inner meningeal layer). It extends from foramen magnum to the lower border od second sacral (S2) vertebra.
- Arachnoid mater: It also extends from foramen magnum to the lower border od second sacral (S2) vertebra.
- Pia mater: It closely invests the spinal cord and below the spinal cord it continues as a thread like structure called filum terminale , which is attached to the dorsal aspect of 1st coccygeal vertebra.
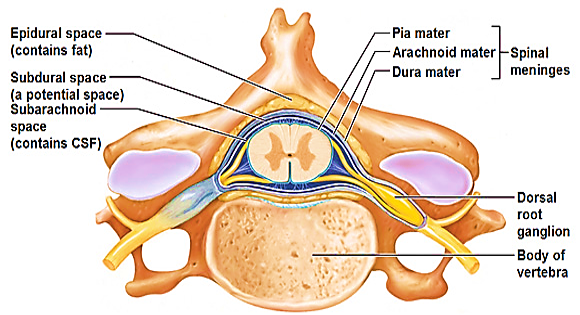
The three space surrounding the spinal cord are:
- Epidural space: it is between the spinal dura mater and the vertebral canal. It contains loose areolar tissue and internal vertebral venous plexus.
- Subdural space: It is a potential between the arachnoid mater and dura mater. It contains a thin layer of fluid.
- Subarachnoid space: it is present between the pia mater and the arachnoid mater and contains cerebrospinal fluid (CSF). Below the termination of spinal cord, the subarachnoid space around the filum terminale internum and cauda equina is more spacious and is called lumbar cistern (from lower border of L1 vertebra till the S2 vertebra). The lumbar puncture is done here to obtain CSF.
Applied Aspects
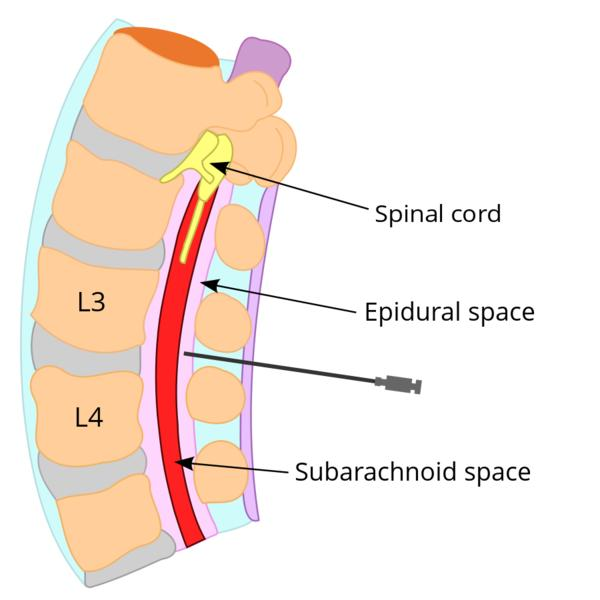
Lumbar Puncture
It is done to obtain the CSF from the subarachnoid space for diagnostic purpose or to inject medicines for therapeutic purpose. It is done below the level of termination of spinal cord to avoid injury to it. The preferred sites are the interspinous spaces between the L3 and L4 or between L4 and L5 vertebrae. The spine of L4 vertebra is located along the imaginary line joining the highest points of the iliac crests.
Epidural block
Anesthetic agent can be injected into the epidural space below the L3 vertebral level, this procedure is called caudal block (epidural block).
What are ligamentum denticulata and what is their clinical significance?
Ligamentum denticulata (single-denticulatum):
- They are two ribbon like longitudinal bands of pia mater extending from the lateral aspect of spinal cord to the duramater. Their main function is to stabilize the spinal cord within the vertebral canal.
- Each band lies on each side between the dorsal and ventral nerve roots.
- Their lateral margin along the attachment to dura mater has 21 teeth-like projections.
- The first tooth of each ligamentum denticulatum is at the level of the foramen magnum, while the last tooth is forked and lies between T12 and L1 spinal nerves.
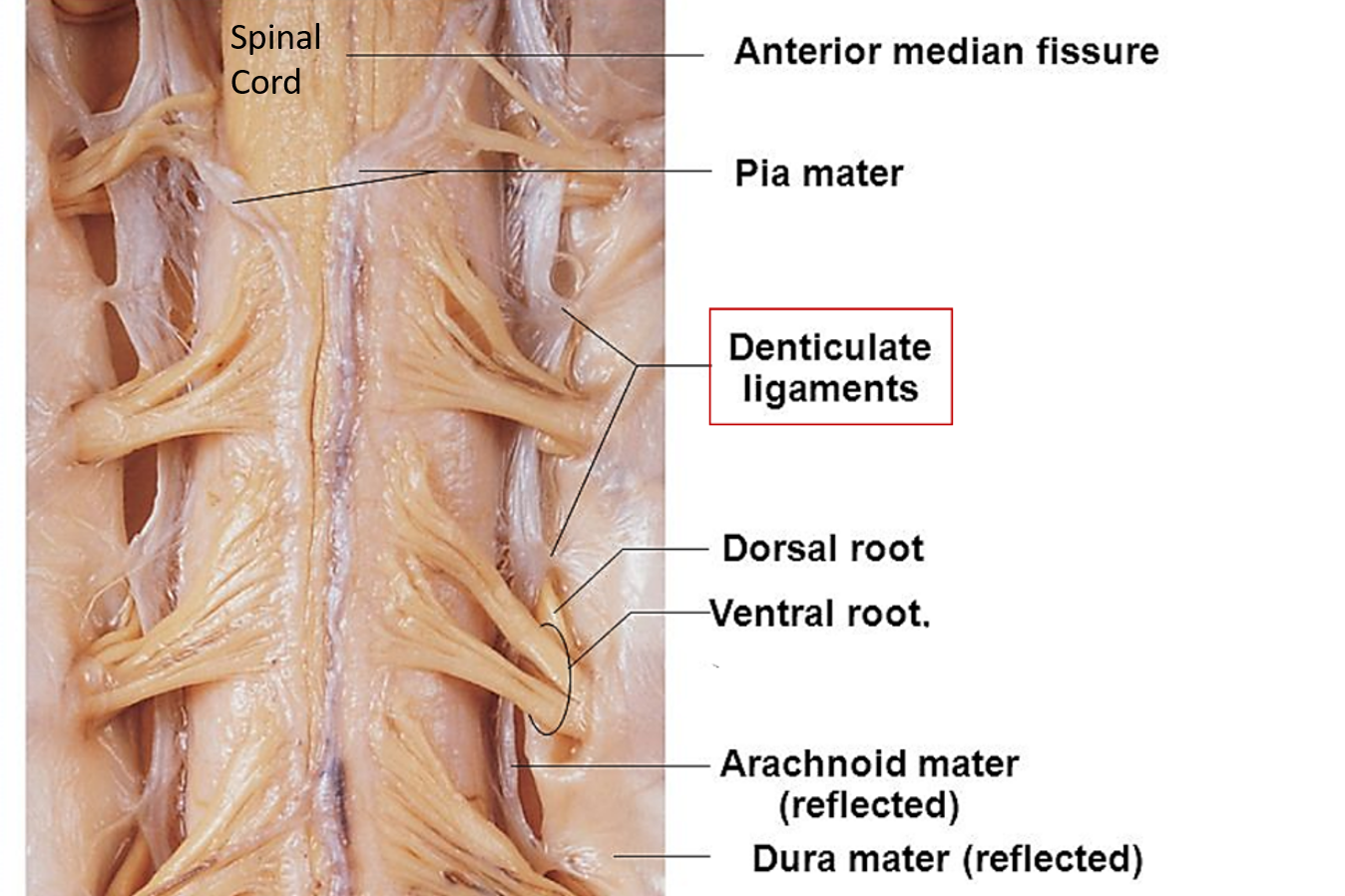
Applied Aspect
The posterior root of L1 spinal nerve lies on the last tooth of ligamentum denticulatum. This serves as a surgeon’s guide to first lumbar nerve, using which the other spinal nerves can be identified in the lower region of spinal cord.
Define Spinal Segment . How many spinal segments are present? Write the vertebral levels of spinal segments
Definition: Spinal segment is that part of the spinal cord which provides attachment to a pair of spinal nerves.
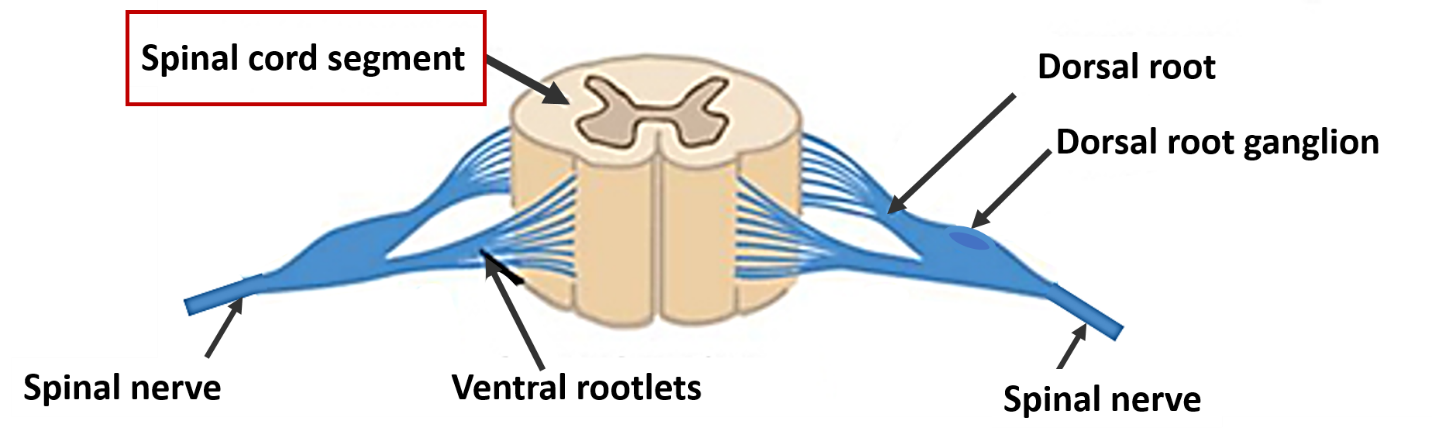
Number of spinal segments: The spinal cord is divided into the following 31 segments. There are:
- 8 cervical segments
- 12 thoracic segments
- 5 lumbar segments
- 5 sacral segments
- 1 coccygeal segment
Approximate vertebral levels of spinal segments:
| Region | Spinal Segment | Vertebral level | General rule |
| Upper cervical | C2 | C2 | Same level |
| Lower cervical | C6 | C5 | One vertebra above |
| Upper thoracic | T4 | T2 | Two vertebra above |
| Lower thoracic | T12 | T9 | Three vertebra above |
| Lumbar | L1-L5 | T10-T11 | 3-5 vertebra above |
| Sacral & coccygeal | S1-5, Co1 | T12-L1 | Six -10 vertebra above |
What are spinal enlargements?
The spinal cord presents two fusiform enlargements called cervical and lumbosacral enlargements. The cervical and lumbosacral enlargements are due to the presence of large number of neurons in C5-T1 and L2-S3 spinal segments to supply the upper and lower limbs respectively.
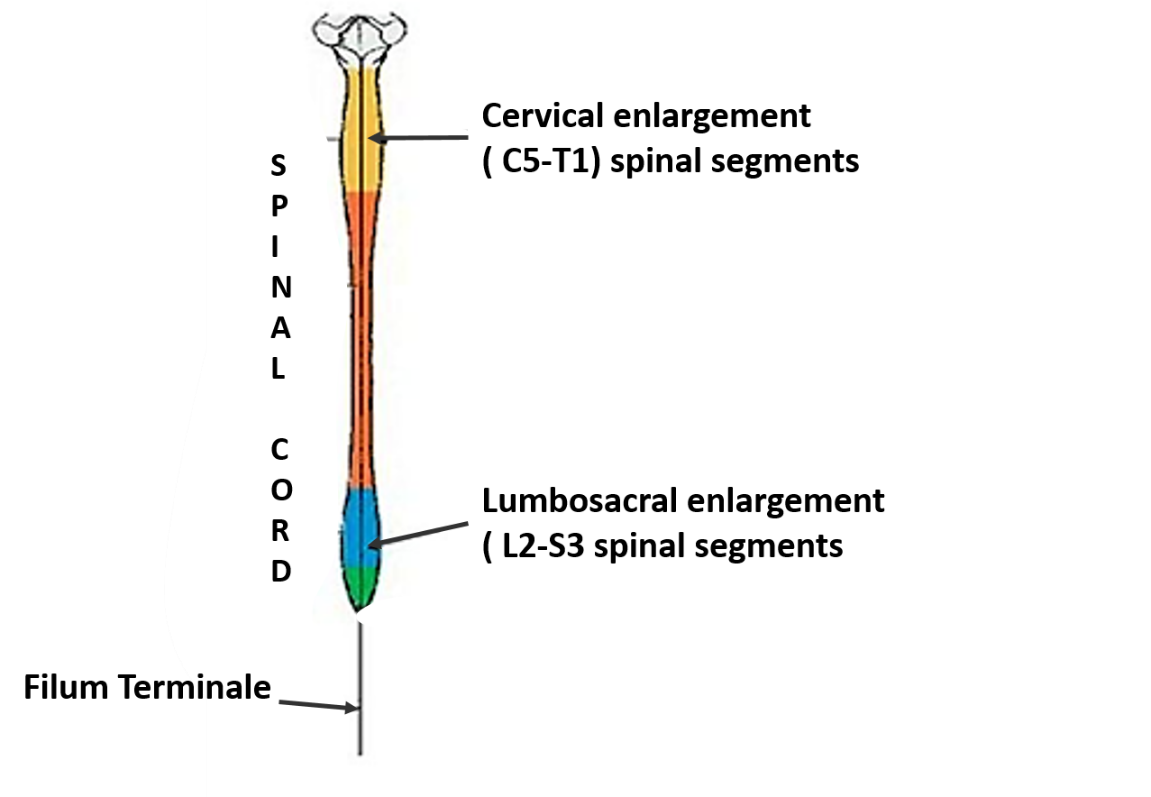
What is Cauda equina?
Cauda equina (meaning tail of horse) is a leash of nerves suspended from the conus medullaris (end of spinal cord). It is composed of L2-L5, S1-S5 and one pair of coccygeal nerves.
Draw transverse section of spinal cord showing the arrangement of grey and white matter.
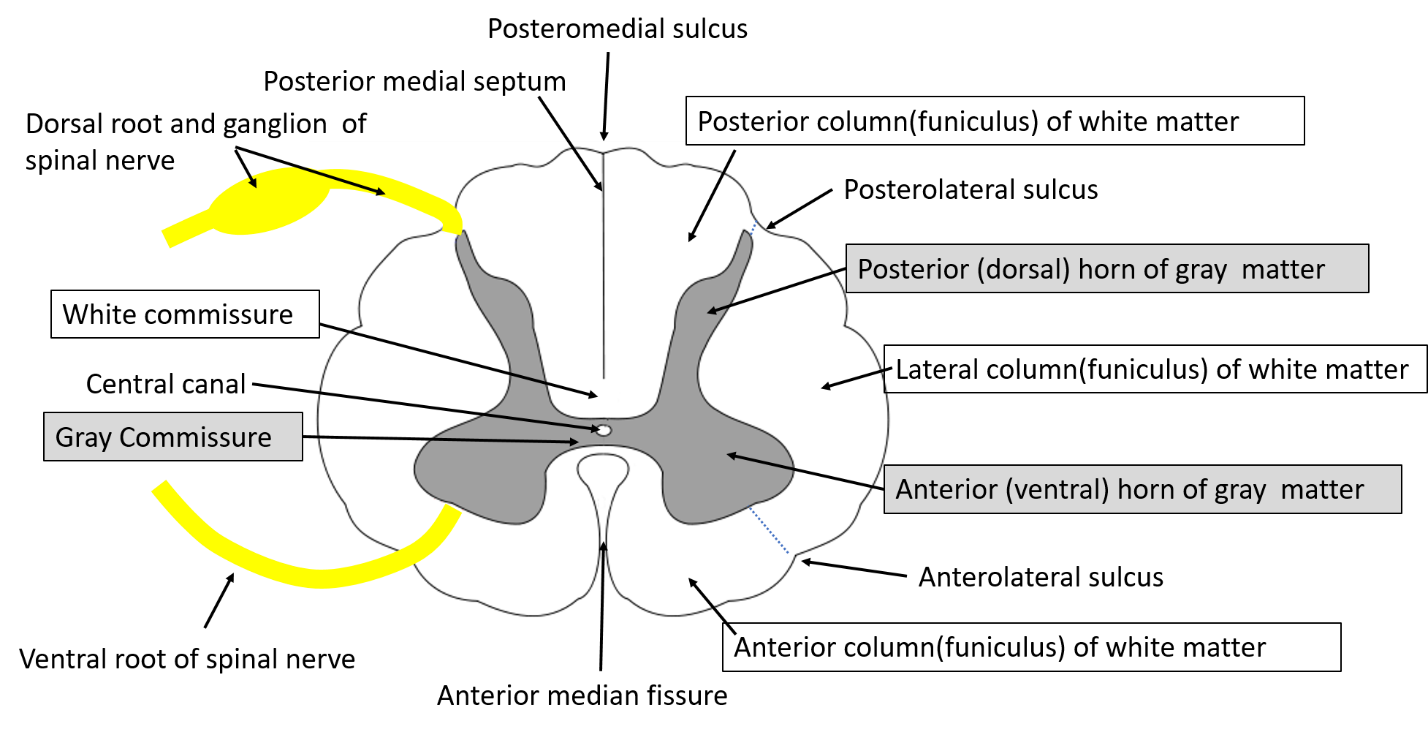
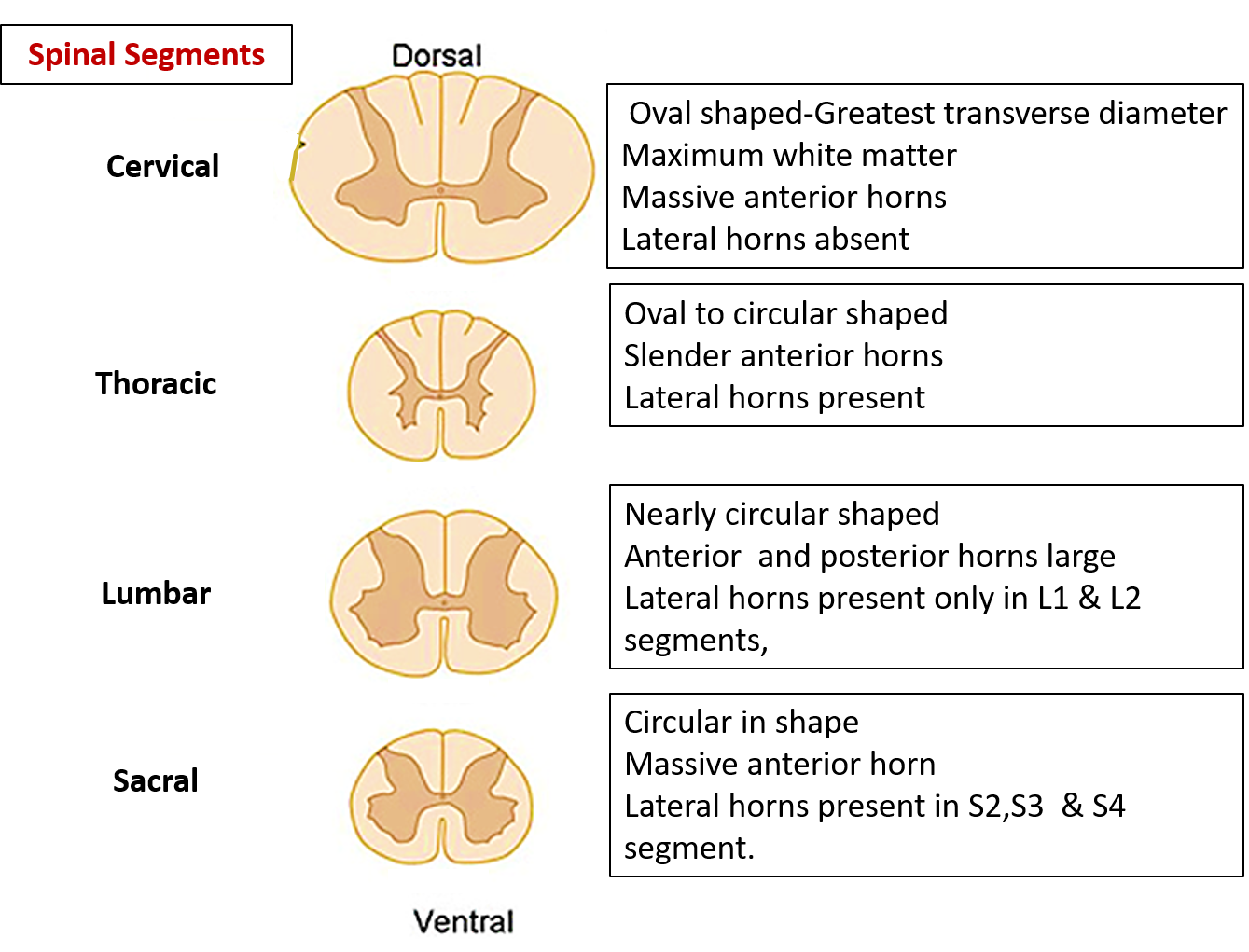
What are the regional differences in the arrangement of white and grey matter in the spinal cord?
The amount of grey and white matter varies in different regions (cervical, thoracic, lumbar and sacral) of spinal cord. Some important points are:
- The amount of white matter increases from sacral to cervical region (ascending (sensory) fibers are added at each level from below upwards coming from upper parts of body and descending fibers (motor) fibers leave white matter to end in anterior horn cells at each level).
- The amount of grey matter is more in the cervical and lumbosacral enlargements because they contain of more neurons to supply upper and lower limbs respectively.
- Lateral horns of grey matter are present in T1-L2 and S1,2,3 spinal segments to accommodate preganglionic neurons for sympathetic and parasympathetic system respectively.
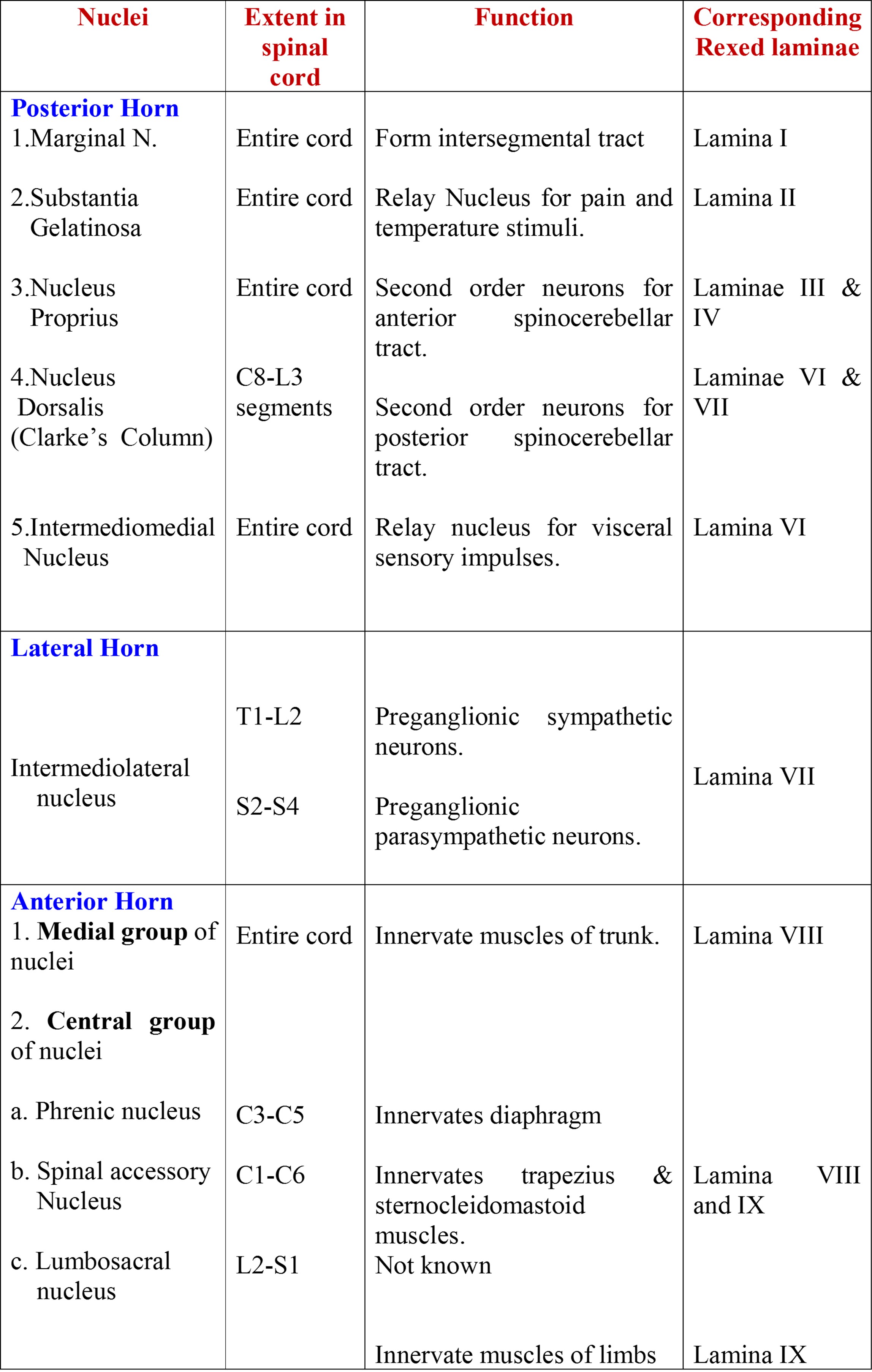
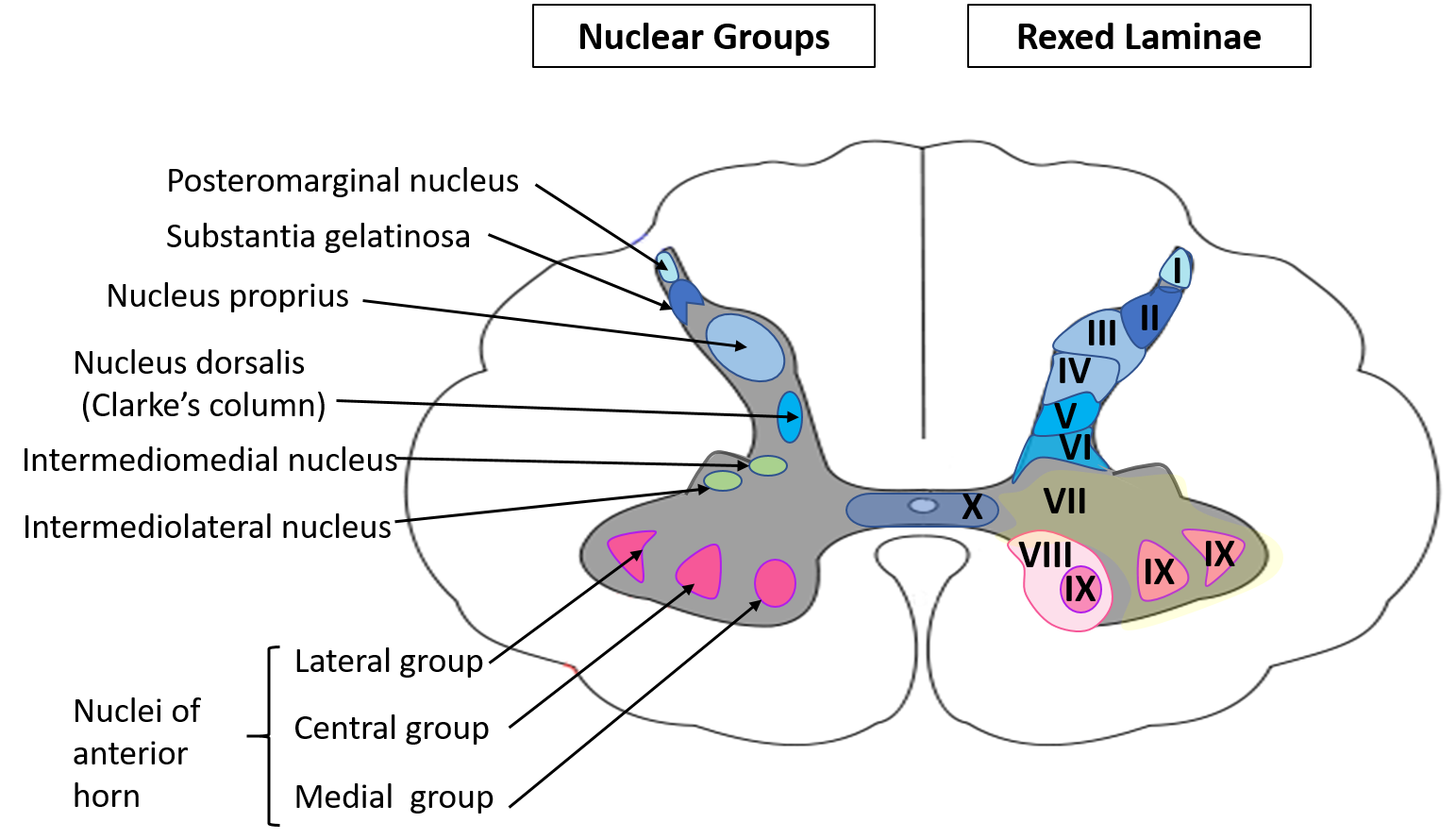
What are the nuclear groups present in the grey columns of spinal cord? What are their function and how do they correspond with the Rexed laminae?
The nuclei in the grey column, their extent in the spinal cord, functions and corresponding Rexed laminae are:
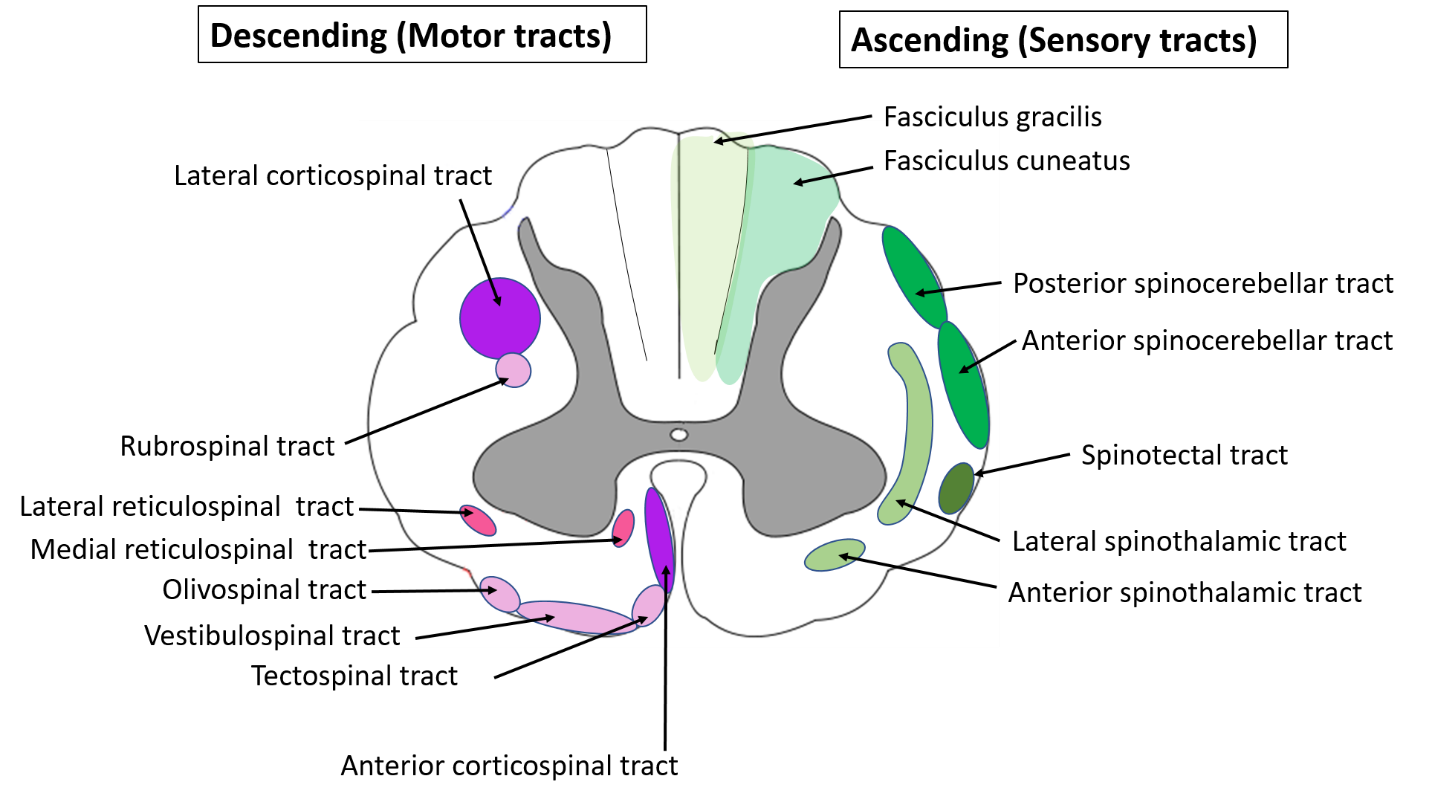
What are the major ascending (sensory) tracts, their location and the sensations carried by them?
The major ascending (sensory) tracts, their location and sensations carried by them are:
| Ascending tract | Location in Spinal Cord | Sensations carried |
| Spinocerebellar tracts 1. Anterior (ventral) spinocerebellar tract 2. Posterior (dorsal) spinocerebellar tract | Anterior column of white matter. Lateral column of white matter | Unconscious proprioception |
| Spinothalamic tracts 1. Anterior (ventral) spinothalamic tract 2. Lateral spinothalamic tract | Anterior column of white matter. Lateral column of white matter | Light touch & pressure, tickle, itch Pain & temperature |
| Posterior column tracts 1. Fasciculus gracilis 2. Fasciculus cuneatus | Posterior column of white matter. | Conscious proprioception. Fine touch, Tactile localization, Two point discrimination, Stereognosis |
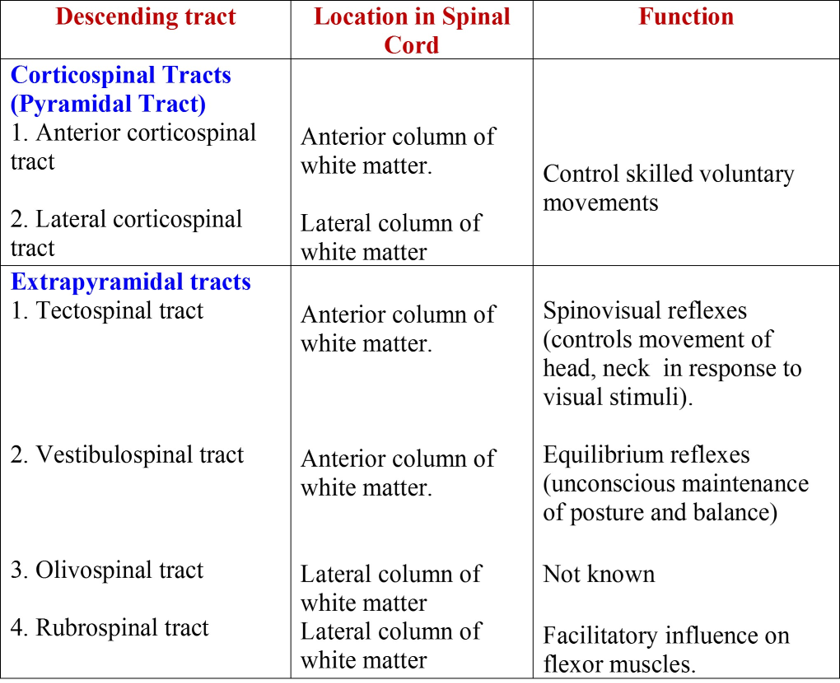
What are the major descending (motor) tracts, their location and the functions?
The major descending (motor) tracts, their location and functions are:
Draw transverse section of spinal cord showing the location of ascending and descending tracts.
Describe the arterial supply of spinal cord.
As the spinal cord is a long structure, it receives its arterial supply from many arteries. Following arteries supply the spinal cord.
- Main arterial supply is by three branches of vertebral arteries:
- One anterior spinal artery
- Two posterior spinal arteries
- It is reinforced by spinal branches of segmental arteries (ascending and deep cervical arteries, posterior intercostal arteries and lumbar arteries) that enter the vertebral canal through the intervertebral foramina.
Anterior Spinal Artery: is formed by the union of two arteries, which arise from the vertebral artery. It descends in the anterior median fissure. Branches from the anterior spinal artery supply the anterior two-thirds of the spinal cord.
Posterior Spinal Arteries: arise either from the vertebral arteries or from the posterior inferior cerebellar arteries. Each artery descends along the posterolateral sulcus and supply the posterior one-third of the spinal cord.
Segmental Spinal Arteries: segmental arteries are branches of ascending and deep cervical arteries (in neck), posterior intercostal arteries (in thoracic region) and lumbar arteries (in lumbar region). Each spinal branch of segmental artery divides into anterior and posterior radicular arteries that accompany the anterior and posterior nerve roots to the spinal cord. They anastomose with the branches of anterior and posterior spinal arteries on the surface of spinal cord.
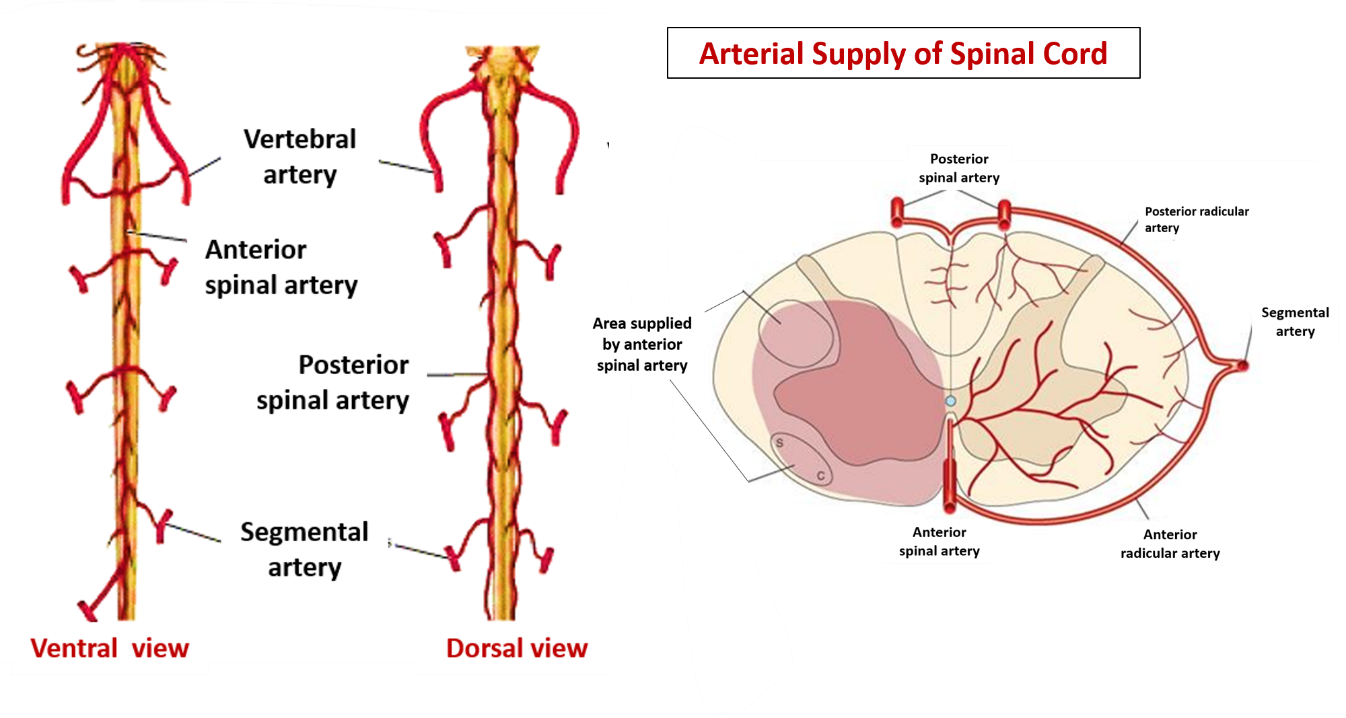
One of the radicular arteries is very large and is called arteria radicularis magna (artery of Adamkiewicz), which arises from the aorta usually on the left side in the lower thoracic or upper lumbar vertebral levels. The importance of this artery lies in the fact that it may be the major source of blood to several segments of spinal cord.
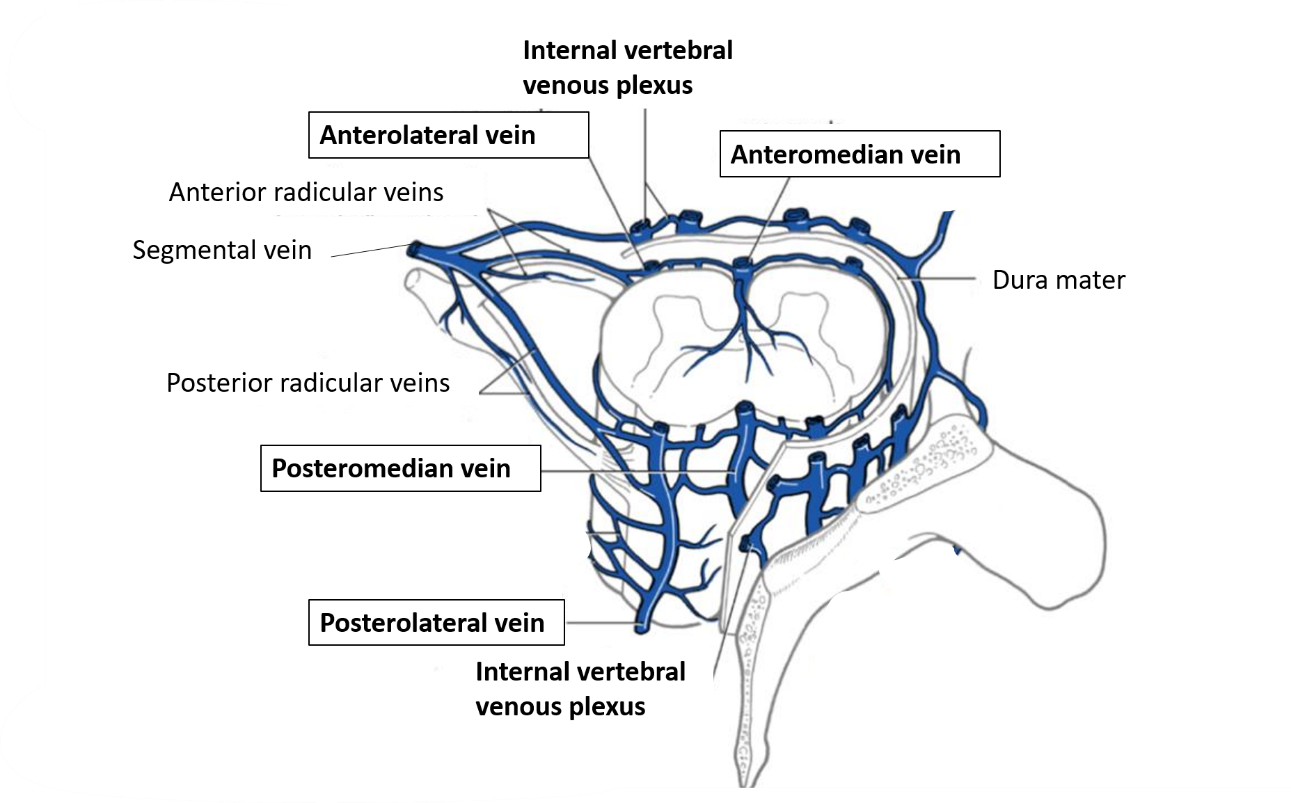
Describe the venous drainage of spinal cord.
The veins of the spinal cord drain into six tortuous longitudinal channels which drain mainly into the internal vertebral venous plexus. The internal vertebral venous plexus communicates superiorly with the basilar plexus of veins in the cranial cavity and is drained by veins that leave through the intervertebral foramina to empty into the vertebral, posterior intercostal and lateral sacral veins.
Applied Aspects – Spnal cord lesions
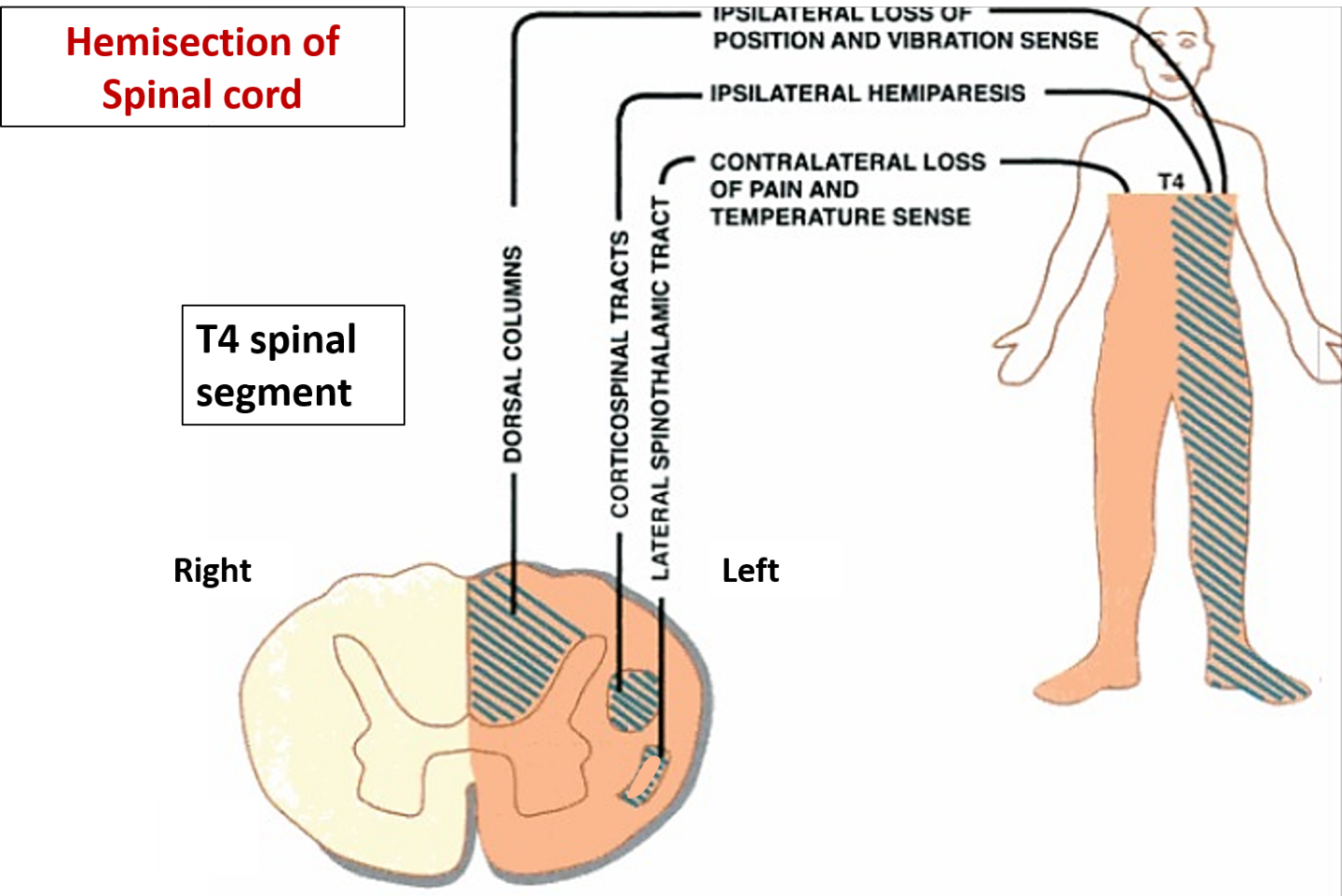
Hemisection of spinal cord (Brown-Sequard syndrome)
| Signs and symptoms Of Brown-Sequard Syndrome | Anatomical basis of Brown-Sequard Syndrome |
Below the level of lesion
|
|
At the level of lesion
|
|
UMN – Upper motor neuron LMN – lower motor neuron
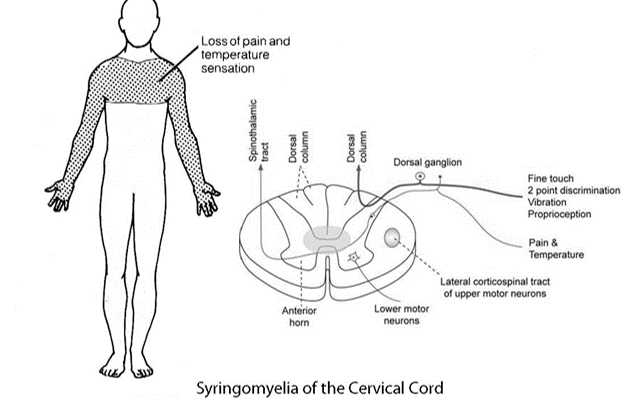
Syringomyelia
It is a degenerative disease of grey and white commissure due to cavitation, which causes enlargement of the central canal.
| Signs and symptoms of Syringomyelia | Anatomical basis of Syringomyelia |
Dissociated sensory loss
|
|
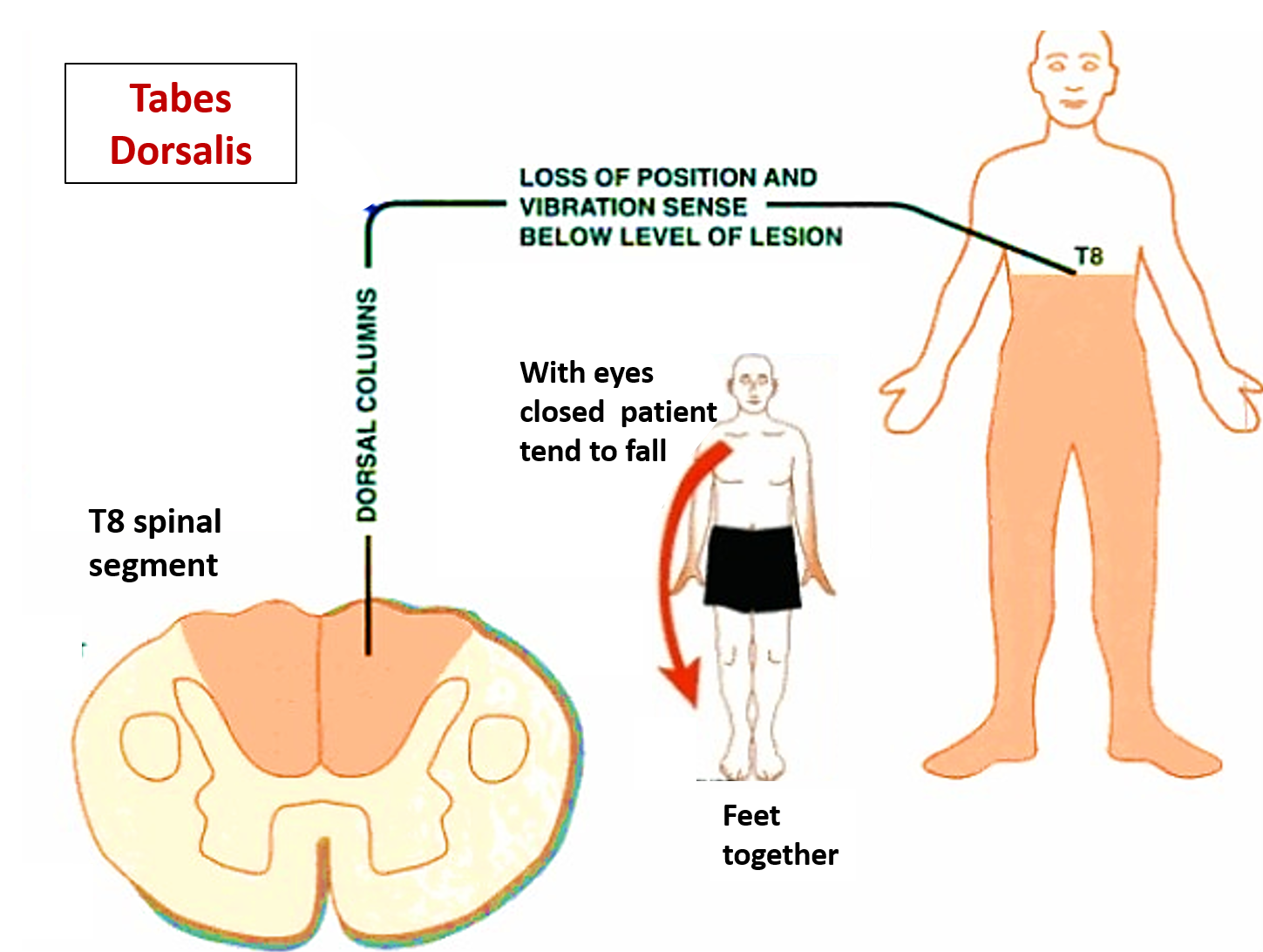
Tabes Dorsalis
It is syphilitic degenerative lesion of posterior column tracts and posterior nerve roots.
| Signs and symptoms of Tabes Dorsalis | Anatomical basis of Tabes Dorsalis |
|
|
Nice
its awesome
thank u
Best ever